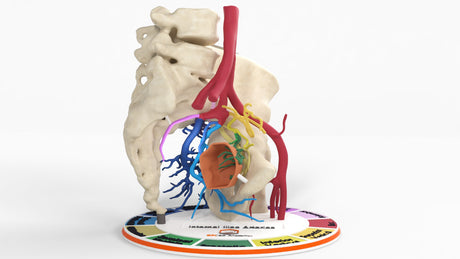
Anatomy:
Internal Iliac Arteries: The aorta, the largest blood vessel in the body, descends through the chest into the abdomen and pelvis, ending in a bifurcation at L4 into the left and right common iliac arteries. The common Iliac artery further divides at the lumbosacral junction into the internal iliac artery, supplying blood flow to the pelvis, perineum, and buttocks, and the external iliac artery continues as the femoral artery supplying blood to the leg. The internal iliac has one of the most complex vascular branching patterns in the body, making it difficult to learn due to high branching variability, anterior and posterior divisions, and the number, size, and variable course of each branch. The branches of the internal Iliac artery supply blood to pelvic organs, including the bladder, reproductive organs, prostate, vagina, part of the rectum, pelvic musculature, and perineum. The Internal Iliac artery branches are divided into anteriorly and posterior divisions.
Divisions of the Internal Iliac Arteries:
Anterior Divisions:
- Umbilical artery: In fetal circulation, it carries deoxygenated blood to the placenta. In adults, the proximal portion remains and gives rise to the superior vesicular artery, which supplies blood to the bladder. The distal fetal portion becomes the umbilical ligament.
- Obturator artery: Travels along the lateral pelvic wall and exits through the obturator foramen, supplying the medial thigh musculature, femoral head, and hip joint. The obturator artery has the largest variability, with 2/3 originating from the anterior division of the internal iliac artery and 1/3 having variant origin, most commonly from the external iliac artery. This has led to significant interest in this artery from surgeons, radiologists, and anatomists due to the importance of early recognition surgically or during embolization, as it can be unexpectedly injured or a missed cause of hemorrhage during angiography. Variation in origin is two times higher in males than females.
- Inferior Vesicular Artery: Males Supplies the inferior bladder, seminal vesicles, and vas deferens
- Inferior Vaginal Artery: Women Supplies to the inferior bladder and vagina.
- Middle Rectal Artery: Supplies the rectum anastomosing with the superior rectal artery (from the inferior mesenteric artery) and inferior rectal artery (from the internal pudendal artery). In men, it supplies the prostate anastomosing with the inferior vesicular artery. In women, the vagina anastomosing with the vaginal artery.
- Internal Pudendal Artery: Exits the pelvis through the greater sciatic notch below the piriformis muscle, then curves around the sacrospinous ligament near the ischial spine and reenters the lesser sciatic foramen to supply the perineum and external genitalia. It travels along Alcock’s canal along the lateral wall of the ischial rectal fossa, playing several vital roles in urinary and bowel continence, erectile function, and sexual health.
- Inferior rectal artery: supplies the anal sphincter and lower rectum.
- Perineal artery: supplies the perineum, in men the scrotum, and in women the labia. Supplies the dorsal artery of the penis.
- Inferior Gluteal Artery: Largest terminal branch of the anterior division of the internal iliac artery. There is significant variability, but most commonly, it extends through the greater sciatic foramen inferior to the piriformis muscle and supplies the skin and muscles of the gluteal region. 70-80% of the time, it is the terminal branch of the anterior division, but in 15-20 % of cases, it can have a common origin with the superior gluteal artery. 5% of the time, it can originate from the pudendal artery and very rarely from the external iliac artery.
- Blood Supply to the Prostate: There is high variability in the origin of the blood supply to the prostate with five main variants.
- Type 1: Inferior Vesicular Artery 35-40%
- Type 2: Internal Pudendal Artery 25-30%
- Type 3: Common trunk with middle rectal artery 20-25%
- Type 4: Obturator Artery 5-10%
- Type 5: Aberrant (external iliac/superior vesicle) 5-10%
Posterior Division:
- Iliolumbar Artery: Supplies the Iliacus Muscle, Psoas Muscle, Quadratus lumborum, and lumbar vertebral bodies. Aids in collateral circulation between internal iliac arteries and lumbar arteries. Despite its small size, the iliolumbar artery has significant clinical importance in trauma, surgery, orthopedics, and interventional procedures. It helps maintain collateral circulation if internal iliac occlusion or surgical ligation is necessary. Posterior screw fixation with pedicle screws at L5 can cause bleeding that is difficult to control through that access point due to its deep location. It can serve as a pathway for treating type II endoleaks of previously treated aortic aneurysms.
- Lateral Sacral Artery: (Superior and Inferior): Supplies the sacrum, spinal meninges, and sacral nerve roots. Passes through the sacral foramen. Pelvic trauma and sacral fractures can be the source of bleeding. During tumor embolization involving the sacrum, the radiologist should be aware of the branching patterns and origin of the lateral sacral artery. Provides collaterals distally if internal artery is occluded or ligated.
- Superior Gluteal Artery: Largest branch of the posterior division. Exits the greater sciatic foramen above the piriformis muscle. Supplies the gluteal muscles. It serves as a vascular supply for many gluteal vascularized flaps used during reconstruction procedures. It has variant anatomy but less so than the internal iliac artery.
Clinical Relevance:
The internal iliac artery is the major blood supply to the pelvis, gluteal region, perineum, and medial thigh. Due to its complex branching pattern and anatomical variations, diseases affecting the internal iliac artery pose significant challenges in surgical specialties and interventional procedures. Angiographic and surgical anatomy is difficult to teach, and it takes years of experience to possess full competency in this area. The radiologist and surgeon should be aware of the various branching patterns and origins and study preprocedural cross-sectional imaging, if available, to avoid unnecessary complications and rapidly treat traumatic hemorrhage. The internal iliac artery can be affected by atherosclerosis and stenosis, resulting in claudication, sexual dysfunction, continence issues, and erectile dysfunction treated with recanalization and occasionally stenting. Aneurysms as the result of previous trauma, surgery, or congenital syndromes can occur along the internal iliac artery and its branch points and are treated surgically or through interventional radiology. In high-velocity injuries and complex pelvic fractures, massive life-threatening hemorrhages can occur. The superior gluteal artery, pudendal artery, and obturator artery are most commonly involved, leading to hemodynamic instability or sciatic nerve compression. Interventional radiologists must quickly assess the site of bleeding during angiography and embolize the correct artery at a site distal enough not to cause unwanted complications such as impotence or incontinence, requiring a firm grasp of the anatomy. Orthopedic surgeons must avoid these arteries during pelvic fixations. Ob/GYN surgeons must be aware of the branching patterns and anatomy to address post-partum hemorrhage and prevent unwanted complications during hysterectomies quickly. Embolization procedures for prostatic enlargement or hypervascular fibroids can lead to sexual and incontinence complications if a firm understanding of the anatomy is not grasped. Similarly, pudendal artery entrapment release and harvesting of gluteal vascular flaps require a deep understanding of the anatomy. 3D models such as this allow the learning physician to have a firm grasp of patient-specific anatomy and branching patterns but also serve as a life-size physical 3D teaching tool with the added benefit of haptic perception.